Myocardial Perfusion Imaging
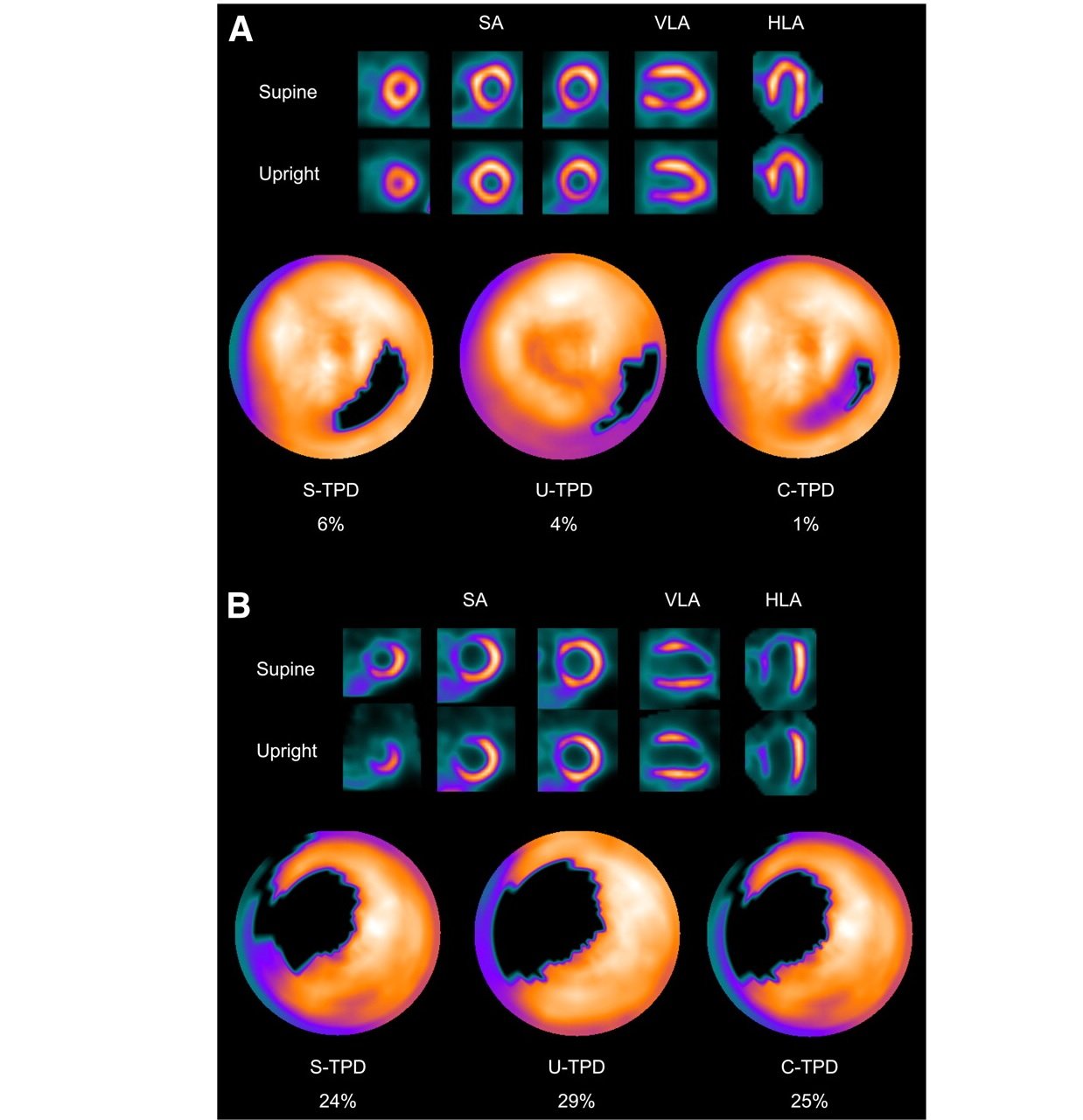
Single-photon emission computed tomography (SPECT) is a nuclear medicine topographic imaging technique that uses gamma rays to provide 3-dimensional (3D) cardiac images. The study offers detailed information about cardiac perfusion and function including wall motion, wall thinkenning and ejection fraction

Device summary. To acquire single-photon emission computed tomography (SPECT) images, the patient lies still in a supine position, and the gamma camera is rotated around the patient. Courtesy of Patrick J. Lynch, Yale University
SPECT is based upon the flow-dependent and/or metabolism-dependent selective uptake of a radioactive tracer by functional myocardial tissue. This method was developed to evaluate myocardial perfusion and viability and is applied both at rest and after exercise or pharmacologic stress to assess inducible ischemia due to flow limiting coronary stenoses
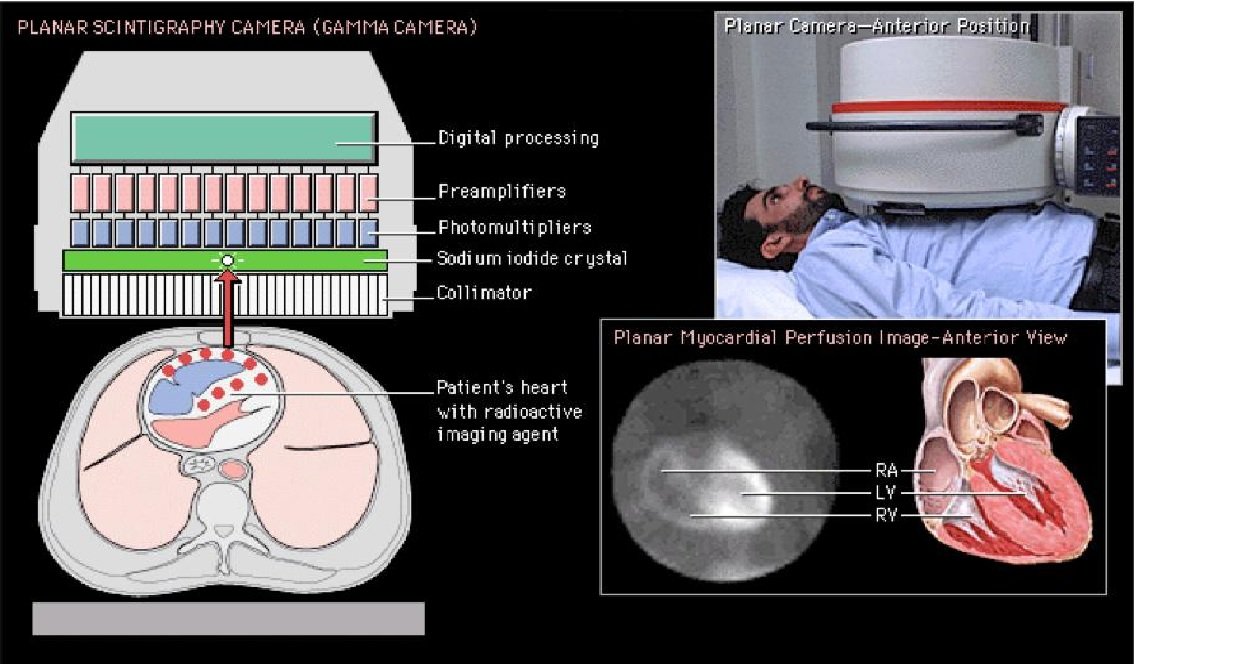
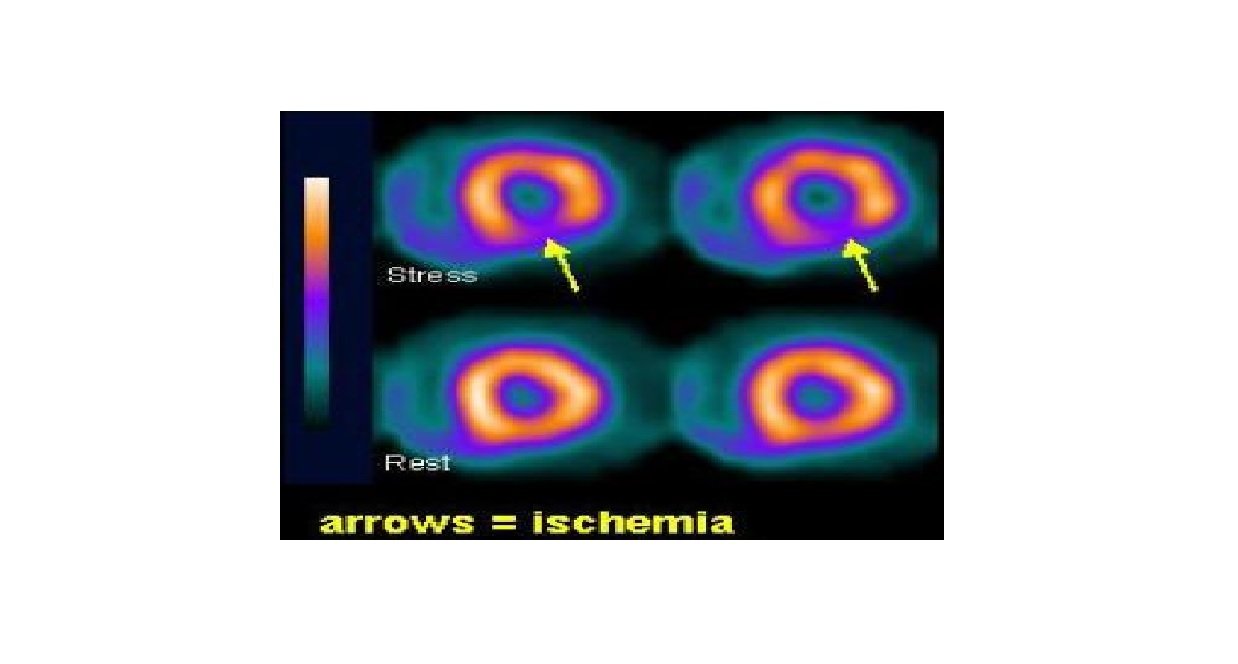
The underlying principle is that under conditions of stress, the diseased myocardium receives less blood flow than normal myocardium. SPECT imaging performed after stress reveals the distribution of the radiopharmaceutical, and therefore the relative blood flow to the different regions of the myocardium. Comparing stress images to a further set of images obtained at rest aids in diagnosis. See the following image
The technique involves the intravenous injection of small amounts of radioactive tracer (gamma-emitting radioisotope), which is avidly taken up by the cardiomyocytes so that the initial myocardial tracer distribution is in proportion to the viable myocardium
Images taken during dynamic exercise or pharmacologically induced stress (using vasodilators such as adenosine or beta-agonist such as dobutamine) and rest injections enable independent assessment of myocardial perfusion and viability
Gated Imaging
ECG-Gated Imaging offer accurate functional parameters of the heart, including cardiac volumes (EDV,ESV), wall motion, wall thikenning and of course Ejection Fraction. Evaluation of the left ventricular (LV) function is important in clinical cardiology. Quantifying the degree and extent of the LV functional abnormalities permits a systematic assessment of the disease process on the myocardial performance, provides an objective basis for the risk stratification and therapeutic strategy, and allows for the sequential follow-up of the therapeutic response
Indications
In patients who present with acute, stable chest pain, SPECT has been shown to be more cost-effective than any other diagnostic modality to date[] and more accurate than exercise ECG in detecting myocardial ischemia. Special indications include determination of the hemodynamic significance of anomalous coronary arteries[]and muscle bridging[] and coronary aneurisms in the setting of Kawasaki disease
Inferior and posterior abnormalities and small areas of infarction can be identified, as well as the occluded blood vessels and the mass of infarcted and viable myocardium
In patients with known CAD, SPECT has been proven the single more powerful technique in predicting the likelihood of future cardiac events
Assessment of viable myocardium in a specific coronary artery distribution after a heart attack: Stress images in SPECT may help determine the degree of inducible ischemia or viable myocardium that are amenable to revascularization
Post intervention revascularization (coronary artery bypass graft or angioplasty) evaluation
Radiation exposure
Myocardial perfusion imaging has nowdays an average effective dose of 6 mSv. According to a study by Einstein et al, new high-efficiency (HE) cameras with specialized collimators and solid-state cadmium-zinc-telluride detectors offer the potential to maintain image quality while reducing the radiation dose. They found that ultra-low-dose high-efficiency SPECT (ULD HE SPECT) rest imaging correlates highly with standard-low-dose (SLD) A-SPECT. ULD HE SPECT was shown to have improved image quality, to have comparable extracardiac activity, and to achieve radiation dose reduction to 1 mSv for a single injection
Dr Ibrahim Al Butaihi
Consultant Nuclear Medicine & Functional Imaging, Maasstad Hospital
Rotterdam, The Netherlands